The world of psychedelics is indeed changing, and Nushama’s approach is a testament to that shift. Gone are the days when psychedelic therapy was relegated to underground circles or stigmatized as purely recreational. Places like Nushama are redefining the conversation, blending clinical rigor with an atmosphere that feels more like an immersive art installation than a sterile medical facility. It’s a far cry from the dimly lit basements or rave scenes where ketamine once thrived—now, it’s administered in serene, thoughtfully designed spaces aimed at healing.
The Science Behind Ketamine’s Resurgence
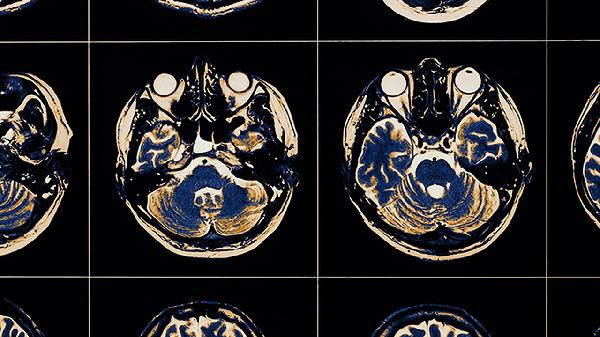
Ketamine’s journey from anesthetic to party drug to mental health treatment is nothing short of fascinating. Initially synthesized in the 1960s, it was quickly adopted in medical settings for its ability to induce anesthesia without suppressing breathing—a game-changer for emergency medicine. But its dissociative and hallucinogenic effects also made it a hit outside the OR. By the '90s, it had cemented its place in club culture, often used for its dreamlike, out-of-body sensations. Yet, even as it gained notoriety as a recreational substance, researchers quietly continued exploring its therapeutic potential. Fast forward to today, and ketamine is having a serious moment in psychiatry. Unlike traditional antidepressants, which can take weeks to kick in (if they work at all), ketamine often produces rapid relief—sometimes within hours. This is huge for people with treatment-resistant depression, a condition that leaves many feeling hopeless after cycling through medications with little success. The key lies in ketamine’s unique mechanism: it targets glutamate, the brain’s most abundant neurotransmitter, which plays a major role in mood regulation and neuroplasticity. By temporarily quieting the brain’s default mode network—the area responsible for self-referential thoughts and rumination—ketamine creates a window for new neural pathways to form. Essentially, it helps the brain hit the reset button.
Why the Setting Matters
Nushama’s dreamy, almost surreal ambiance isn’t just for show—it’s a deliberate part of the therapy. Psychedelic-assisted treatments, whether using ketamine, psilocybin, or MDMA, emphasize the importance of "set and setting." "Set" refers to the patient’s mindset going into the experience, while "setting" is the physical and emotional environment. A calming, aesthetically pleasing space can significantly influence the outcome, helping patients feel safe and open to the introspective journey ketamine facilitates. This isn’t just woo-woo theory; it’s backed by research. Studies on psychedelics consistently show that environment plays a critical role in shaping the therapeutic experience. At Nushama, every detail—from the celestial soundscape to the soft lighting—is designed to minimize anxiety and maximize comfort. Even the choice of artwork, like the mural of intertwined nymphs, serves a purpose: to evoke a sense of wonder and connection, subtly guiding patients toward a more expansive state of mind.
Breaking the Cycle of Depression
For those stuck in the exhausting loop of depression, ketamine offers something rare: a glimpse of possibility. Traditional treatments often focus on managing symptoms, but ketamine therapy aims to disrupt the underlying patterns that keep people trapped in negative thought cycles. Dr. Radowitz explains it like this: "Imagine your brain is a ski slope. Over time, deep grooves form where your thoughts consistently go—usually down the same negative trails. Ketamine is like a fresh snowfall, covering those grooves so new paths can be carved." This isn’t a one-and-done fix, though. Most patients undergo a series of sessions, often paired with integration therapy to help them process insights gained during the experience. Think of it as mental spring cleaning—ketamine shakes things up, and therapy helps you reorganize. The goal isn’t just temporary relief but lasting change, which is why clinics like Nushama emphasize a holistic approach, combining medical oversight with psychological support.
The Legal and Ethical Landscape
Despite its promise, ketamine therapy exists in a legal gray area. While the FDA has approved a ketamine-derived nasal spray (Spravato) for treatment-resistant depression, intravenous ketamine remains off-label. This means clinics like Nushama operate under physician discretion, which has led to some controversy. Critics argue that the lack of standardized protocols raises concerns about safety and consistency, while advocates counter that strict regulations would limit access for those who desperately need alternatives. Then there’s the cost barrier. Since most insurance plans don’t cover ketamine infusions, a full course of treatment can run thousands of dollars—putting it out of reach for many. This raises ethical questions about equitable access, especially when early adopters tend to be wealthier, urban populations. As the field evolves, finding ways to make these therapies more affordable and inclusive will be crucial.
What’s Next for Psychedelic Medicine?
Ketamine is just the beginning. The resurgence of interest in psychedelics has sparked a wave of research into other substances, like psilocybin (found in "magic mushrooms") and MDMA, both of which are in late-stage clinical trials for conditions like PTSD and major depression. The success of clinics like Nushama signals a broader cultural shift—one where psychedelics are increasingly seen as legitimate tools for healing rather than relics of counterculture. Still, challenges remain. Stigma lingers, and misconceptions about these substances persist. But as more people share their transformative experiences and more data emerges, the narrative is changing. The future of mental health treatment might just involve more cherry blossom murals, celestial playlists, and yes, those white chairs—because if there’s one thing the psychedelic renaissance teaches us, it’s that healing doesn’t have to look clinical to be effective.
The psychedelic landscape is evolving, and with it, our understanding of mental health care. Nushama’s approach—blending science, art, and intentionality—offers a glimpse into what the future could hold: a world where therapy isn’t just about numbing pain but about awakening possibility. And if that future includes fruit-infused water and pink-hued dreamscapes, well, sign us up.